Retinal Vein Occlusion
Types Risk Symptoms Causes Treatment
A retinal vein occlusion occurs when the circulation of a retinal vein becomes obstructed by an adjacent blood vessel. This results in the stoppage of blood flow, causing hemorrhages in the retina. The retinal veins are the small "pipes" in the retina that drain blood out of the retina, back to the heart. The veins drain the blood out of the eye, while the retinal arteries are the small blood vessels that deliver the blood (from the heart) to the retina.
 Next:
Nutrients for circulatory support.
Next:
Nutrients for circulatory support.
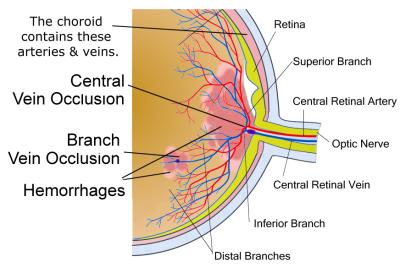 Retinal vein occlusion is second only to diabetic retinopathy as a cause of visual
loss due to retinal vascular disease. There are two forms of retinal vein occlusion,
branch retinal vein occlusion (BRVO) and central retinal vein occlusion (CRVO).
While there are similarities in the pathogenesis and clinical nature of these two
events, each has unique etiologies, differential diagnosis, management and prognosis.
Retinal vein occlusion is second only to diabetic retinopathy as a cause of visual
loss due to retinal vascular disease. There are two forms of retinal vein occlusion,
branch retinal vein occlusion (BRVO) and central retinal vein occlusion (CRVO).
While there are similarities in the pathogenesis and clinical nature of these two
events, each has unique etiologies, differential diagnosis, management and prognosis.
A branch retinal vein occlusion is essentially a blockage of the portion of the eye's circulation that drains the retina of blood.
Types of Occlusion
Eye doctors also categorize retinal vein occlusions based on potential treatment strategies:
Nonischemic (also called venous stasis retinopathy) occlusions are relatively benign and account for 75-80% of all cases. The body develops alternate pathways for blood vessels that may result in macular edema but rarely in neovascularization with its accompanying problems.
Ischemic (hemorrhagic retinopathy) means that there is an inadequate blood supply, resulting in a marked decrease in vision. Hemorrhagic retinopathy results in complications such as macular edema, macular ischemia, and neovascularization that can lead to blindness in two-thirds of people diagnosed with this disorder.
Who is at Risk?
Branch retinal vein occlusions are by far the most common cause of retinal vascular occlusive disease. Males and females are affected equally. Most occlusions occur after age 50, although younger patients are sometimes seen with this disorder (in this age group it is often called papillophlebitis). The highest rate of occurrence is in individuals in their 60's and 70's. The risk factors for this disorder are similar to those for vascular occlusive disease elsewhere in the body such as stroke and coronary artery disease.
Symptoms
Gradual or subtle vision loss. The severity of vision loss may depend on where the blockage or clot occurs. In some cases, this loss of vision is subtle with intermittent episodes of blurred vision.
Sudden vision loss. In other cases, vision loss may be sudden and dramatic, particularly related to those with the ischemic form of RVO. A severe blockage in an artery or vein is called an occlusion or stroke.
- Patients with CRVO generally show vision changes. It may present in sudden, painless, monocular vision loss or dense central scotoma (partial loss of vision or blind spot).
- BRVO causes a sudden and painless vision loss. If the affected area is not in the center of the eye, BRVO can go unnoticed without symptoms.
Causes
The majority of causes and risk factors associated with retinal vein occlusion are lifestyle driven, meaning that they can be avoided with healthy lifestyle choices.
The exact process, known as atheroma, or atherosclerosis (hardening of the arteries), is a degenerative disorder linked to the ongoing accumulation of plaque and scar tissue (from the repair of microscopic tears due to high blood pressure) in the arterial walls and the subsequent narrowing and weakening of the walls. As these patches of deposits and scar tissue accumulate, the risk for heart attack and stroke increases, as does the risk for peripheral vascular diseases (PVD), which are marked by degeneration of the blood vessels in areas other than the heart.
Examples of PVD include stroke (brain), renal (kidney) artery disease, venous disease (problems with veins in the legs, including spider and varicose veins), and pulmonary vascular disease (lungs). So, if retinal vein occlusion occurs in a person with cardiovascular concerns, it could be considered a type of PVD.
The risk of developing retinal vein occlusion seems to increase if you have risk factors for cardiovascular disease. These include:
- High blood pressure. According to one study, 73% of patients with CRVO had hypertension, and 23% had diabetes.
- High cholesterol levels. According to a study of patients with central retinal vein occlusion in people 40 years old and younger, hypercholesterolemia (identified in 65% of cases), hypertriglyceridemia (64% of cases), and hyperhomocysteinemia (42% of cases) were identified as risk factors. Three patients (14%) developed stroke, and one (5%) developed transient ischemic attacks during follow-up, suggesting that the presence of CRVO may indicate serious systemic diseases.
Conditions other than cardiovascular concerns that contribute to retinal vein occlusion include:
- Diabetes
- Smoking and glaucoma (both raise pressure in the eye)
- Diseases that promote undesired or abnormal blood clotting, such as antiphospholipid antibody syndrome (APS)
- Aging (not a condition but linked to high risk, particularly if other underlying issues exist)
Conventional Treatment
Unfortunately, there is no way to actually unblock retinal veins. However, your doctor may treat any health problem that seems to be related to the retinal vein occlusion. Currently, anti-VEGF drugs such as ranibizumab and bevacizumab appear to be the most frequently chosen treatment options with little potential for side effects. Steroids are another option but have more potential side effects. Some treatment strategies may use both. According to an article in Review of Ophthalmology, 99% of people who get anti-VEGF injections receive some improvement, at the least. Injections need to be given regularly for one to two years for lasting benefits (in this review, one out of two patients show improved vision).
The aim of treatment is to detect and treat under-lying risk factors, but also to detect and treat complications of the blocked vein, where possible. If an underlying cause such as high blood pressure, high cholesterol, or diabetes is determined, then proactive treatment for these conditions is necessary. Managing secondary effects includes the following procedures:
- Closing leaky blood vessels with laser treatment
- Administering injections of vascular endothelial growth factor (VEGF) that can temporarily resolve the neovascularization, reduce macular edema, and improve vision.
- Intravitreal injection of corticosteroid drugs to combat the inflammatory components that leads to edema (steroid implants are now also being used)
- Focal laser therapy to reduce swelling due to edema
- Pan-retinal photocoagulation therapy when patients have new blood vessel formation following the retinal vein occlusion
Also, the doctor may prescribe medications for lowering cholesterol or controlling high blood sugar that is related to diabetes, etc. Early diagnosis and treatment of retinal vein occlusion, and any complications, may make a difference to the level of visual loss in the short and long run.
Complementary Approach
Because this disorder is largely related to lifestyle choices, preventive measures such as stopping smoking, exercising regularly, eating a healthy diet, losing weight if you are overweight, keeping blood pressure and cholesterol at healthy levels, and managing chronic stress are all exceedingly helpful in preventing or avoiding this disorder. These lifestyle choices support healthy circulation, help to keep the blood vessels unclogged, and support the free flow of essential nutrients to the retina. The goal is to maintain healthy vision as well as reduce the risk of future occurrences through proper medical and lifestyle management.
 Next:
Nutrients for circulatory support.
Next:
Nutrients for circulatory support.
Diet & Nutrition
- Prevention is important: diet, exercise, not smoking, managing stress are all essential.
- Avoid nutritional deficiencies
- Support prevention with complementary medicine along with traditional medicine
- Certain nutrients such as zeaxanthin, lutein, gingko biloba, omega-3 fatty acids, bilberry and a number of other vitamins and enzymes may help preserve vision for those who are at risk of or have had experienced a Retinal Vein Occlusion.
- Some research indicates that daily use of Microcurrent Stimulation may help preserve vision as well.
- See nutrients to support eye vascular health
Lifestyle & General Health
- Eliminate smoking. Smoking produces cyanide, a retinal toxin.
- Limit the amount of medications as much as possible but be sure to work closely with your health provider.
- Exercise daily - engage in at least 20 minutes of aerobic exercise every day, such as walking and swimming.
- Care for your emotional health It is important for maintaining physical health. Take up the practice of yoga, meditation, tai chi, walks outdoors or prayer on a daily basis.
Retinal Occlusion News
Want to learn more? See our blog for news on retinal occlusions.
 See
Vitamins & Supplements to support the eye
vascular system and overall eye health.
See
Vitamins & Supplements to support the eye
vascular system and overall eye health.
Related Conditions
There are other conditions that either have similar conditions, or are due to similar causes, or respond to similar treatments.
Neovascular glaucoma. As a result of the body's natural attempt to restore blood drainage to the eye, neovascularization (new blood vessel formation) results in neovascular glaucoma.
Neovascular glaucoma begins first with the new blood vessels forming in the iris or the angle where the iris meets the cornea.
According to a 2004 study, the overall prevalence of glaucoma was 9.9% and the prevalence of ocular hypertension was 16.2% for those with central retinal vein occlusion and hemi-occlusion involving approximately half of the retina.
Vitreous hemorrhage can also occur due to occlusion of retinal veins.
Retinal detachment can develop in late or severe cases of retinal occlusion.
Macula edema may develop in patients with the relatively benign non-ischemic type of occlusion.
Retinal artery occlusion, in which an artery, rather than a vein is blocked.
 info@naturaleyecare.com
info@naturaleyecare.com



 Home
Home


 Vision
Vision Vision
Vision



 Health
Health Health
Health Research/Services
Research/Services Pets
Pets About/Contact
About/Contact


