Epiretinal Membrane (macular pucker)
Vitamins/supplements Progression Types Symptoms Causes News
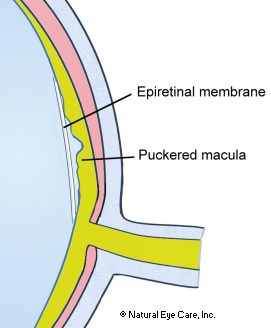
Epiretinal membrane (ERM), also known as macular pucker, is identified with many different terms, including surface-wrinkling retinopathy, cellophane maculopathy, and pre-retinal macular fibrosis. ERM gets its common name from scar tissue that has formed on the macula, creating a very thin, nearly transparent layer of fibrous tissue that spreads across the retinal surface. When this thin fibrous layer contracts, the retinal surface is wrinkled or puckered like wrinkles on a bedspread. Other names come from its similarity in appearance to a layer of cellophane, where folding and puckering has not yet developed.
Progression
Epiretinal membranes do not contain blood vessels. They are comprised of fibrocellular cells: glial cells (cells that surround neurons), retinal pigment epithelial cells (lining tissue cells), macrophages (large white blood cells), fibrocytes (cells that produce connective tissue), and collagen (structural protein in connective tissue). This composite is attached to the retina and contracts, distorting the retina. The degree of visual distortion can vary, depending on the amount of, and the location of, the pucker.
Macular pucker is typically a slow-progressing problem that affects the central vision by causing blurring and distortion. As it progresses, pulling of the membrane on the macula (central part of the retina) may cause swelling. An epiretinal membrane will not cause total blindness and will typically and only affect the central vision in the affected eye. Peripheral or ‘side’ vision remains unaffected. The vast majority of those with ERM are asymptomatic. For most people, vision remains stable and does not get progressively worse. Usually macular pucker affects one eye, although it may affect the other eye later.
 See
Vitamins &
Supplements to support macular health.
See
Vitamins &
Supplements to support macular health.
This condition is seen most in elderly persons over 75 and is often associated with other eye problems such as vitreous or retinal detachment, diabetic retinopathy, trauma to the eye, and other conditions. Based on one study, the prevalence of ERM was 1.9% in persons younger than 60 years of age, 7.2% in persons 60 to 69 years of age, 11.6% in persons 70 to 79 years of age, and 9.3% in persons 80 years of age and older, with slightly higher rates in women. Strong associations were shown for this with diabetes, as well as with past cataract surgery and retinal disease.
Types of Epiretinal Membrane
Idiopathic epiretinal macular membrane (IEMM) is one of the most common forms of epiretinal membrane. Membranes that are comprised of glial cells (cells that surround nerve cells, insulating them) apparently develop spontaneously or from idiopathic (unknown) causes. Posterior vitreous detachment results in 75–93% of these cases.
Retinal detachment-related. This is the other common type of epiretinal membrane in relation to breaks or tears in the retina, detached retina, or surgical reattachment of the retina to the pigmented layer that uses laser photocoagulation and cryopexy. These membranes are mostly comprised of retinal pigment epithelial cells.
Vitreous traction-related (VMT). If there is no posterior vitreous detachment, then patients may experience vitreomacular traction syndrome The vitreous contains millions of fine fibers that are attached to the surface of the retina. As we age (over 50 years old commonly), the vitreous that keeps the shape of the back of our eyes begins to shrink, causing a pulling on the retina.
Interior limiting membrane. Sometimes the interior of the retinal surface is affected, in which case the membrane forms prior to a vitreous detachment.
Symptoms
At first symptoms may not be noticeable, or a very modest reduction in vision acuity may occur. Progression can give rise to distorted vision in which lines in a grid may appear wavy, or parts of the grid may be blank, gradually worsening until there may be distortion and impairment. In some cases macular edema may occur (in which fluid is retained in a cyst under the macula, or retinal detachment (in which the retina separates from the lining of the eye) may develop.
You helped me (via email) a year ago with my retinoschisis and am glad to rapport that my eye is doing quite well! I’ve followed your recommendation to a T and today only see an occasional flash. Even my floaters, though still there, are much less than before. Also the pain from the optic nerve is less frequent and only occasionally will feel it... All in all, it’s been a relief that everything has gone so well so needless to say I am grateful to you!
Ann Marie - May, 2021
Macular Pucker News
Want to learn more? See our blog news on macular pucker.
 See Vitamins & Supplements to
support the macula and retina as well as overall eye health.
See Vitamins & Supplements to
support the macula and retina as well as overall eye health.
Footnotes and sources
1. Mitchell, P., Smith, W., Chey, T., Wang, J.J., Chang, A. (1997). Prevalence and associations of epiretinal membranes. The Blue Mountains Eye Study, Australia. Ophthalmology, Jun;104(6):1033-40
Although the underlying physiological cause may be unique, there may be similarities in terms of nutritional, diet and lifestyle recommendations made by Dr. Grossman for eye conditions that result in similar vision symptoms to those of epiretinal membrane (macular pucker).
See also research for macular degeneration.
 info@naturaleyecare.com
info@naturaleyecare.com



 Home
Home


 Vision
Vision Vision
Vision



 Health
Health Health
Health Research/Services
Research/Services Pets
Pets About/Contact
About/Contact


