Eye Floaters
Why Floaters?
Treatment Symptoms Causes Related conditions
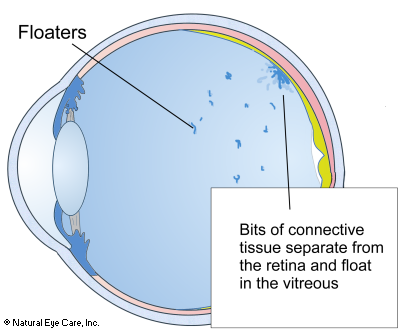
Eye floaters are those small, often irregular, dark shapes that appear on one's field of vision. They are made up of clumps of protein that may look like dots, blobs, strands, cobwebs, etc. Though annoying, they won't harm you and you may not even notice them.
As we age two things begin to happen:
- The vitreous gel that keeps the shape of the back of our eyes starts to liquefy and/or clump and shrink, which creates a pulling on the retina.
- The protein-based connective tissue attaching the vitreous lining weakens, and tiny pieces of connective tissue may float free in the vitreous.
Due to these degenerative changes the incidence of floaters (myodesopsia) in the vitreous humour becomes more prevalent. Light passes through the lens, through the vitreous humour to the retina. We can see floaters because they cast a shadow on the retina. They may look like spots, irregular shapes, or bits of thread that slowly float on the field of vision. We often don't even notice them because they remain "fixed" in relation to the retina because the brain gets used to them and doesn't pay attention to them.
They are generally considered more of a nuisance than a symptom of serious problems unless there is a sudden increase in the number and location of floaters. A ring of floaters to the outside (toward the ears) edge of vision or a sudden increase in floaters is a symptom that should be checked with your ophthalmologist.
 Next:
Nutritional
support, diet, & lifestyle tips for floaters.
Next:
Nutritional
support, diet, & lifestyle tips for floaters.
Symptoms
- Visual spots in the form of specks, strings, clusters, and combinations of these.
- The spots move as you move your eyes.
- The spots tend to drift out of your line of vision when you are not moving your eyes.
- Warning: If you suddenly become aware of new floaters in your vision, see your eye doctor right away to rule out serious problems.
Causes
Age Related. Most vitreous eye floaters are age-related and are due to the vitreous gel gradually liquefying and shrinking or clumping. The vitreous gel helps maintain the shape of the back of our eyes and as it degrades connective tissue (proteins) are released into the gel. More than 50% of people over 70 see them. Some parts of the vitreous may also clump up forming floaters inside the eye. Shrinking of the vitreous that occurs with aging is known as vitreous syneresis.
Near-Sightedness. Those who are nearsighted are also at higher risk of developing eye floaters, particularly if at 6 diopters or over, due to chronic pulling on the retina combined with weakening of the connective tissue to the retina.4 The greater the level of nearsightedness, the higher the risk of vitreous tears and detachments (often resulting in eye floaters), and a higher risk of retinal tears and detachments.
Cataract Surgery. Sometimes complications from cataract surgery can cause floaters. One study assessing types of cataract surgery determined that patients receiving a "hinged capsulotomy" reported fewer floaters.1
Diabetes. Floaters are common in diabetics because that condition causes a number of weak capillaries in the eyes that can leak blood, which can clot and be deposited as floaters in the vitreous.
Eye Trauma. Trauma to the eye may also cause spots and floaters. Many floaters remain in the eye for a long time before they gradually disappear.
Food Allergies. People with food allergies are at higher risk of developing floaters, perhaps because there is poor absorption of nutrients from food and lack of nutrients delivered to the eyes. One paper describes topical drugs applied to the eyes that cause allergic reactions and floaters.6
Candidiasis. Similarly, people with yeast infections may be more at risk of developing floaters, perhaps due to incomplete nutrient absorption.
Prebirth. Floaters may appear in babies during pregnancy as a result of hyaloid artery degradation. Prior to birth, the eyes of the unborn child contain an artery that regresses during the last three months of pregnancy. Sometimes cell material is left behind and is experienced as floaters. Pregnant mothers can take prenatal supplements to help support the development of the baby, along with essential fatty acids for brain development.7
Stress. We believe that chronic stress may contribute to the generation of floaters. Studies show that physical or emotional stress can contribute to the onset of posterior vitreous detachment.5 so developing a daily routine of mediation, yoga, or relaxation is really important.
Kidney Congestion. From the perspective of Chinese Medicine, congestion in the kidney, liver and colon can contribute to development of floaters. The nutrients and herbs we recommend are chosen for their ability to reduce congestion, helping to keep the vitreous free of these little specks and spots. In addition, these supplements help to strengthen the connective tissue of the retina and the strength of the blood veins and arteries.
Vitritis is an inflammation of the vitreous body, which may be caused by a number of viruses such as ocular herpes, cytomegalovirus (related to chicken pox) or other viral infections.
Uveitis. - Inflammation in the uvea in the back of the eye which can be caused by infection, parasites, trauma, a few cancers, and conditions of the immune system.
Cancer A case study reported on a patient with chronic myeloid leukemia who included floaters among his symptoms. 3
Drugs. Some prescription drugs can cause floaters. See "Drugs That Harm the Eyes" for a discussion of medications that could be potentially detrimental to your vision.
Vitreous anomalies. Retinal tears, detachments, leaky blood vessels, and other vitreous anomalies can be experienced as floaters. Note: a full retinal detachment is a medical emergency.
IMPORTANT NOTE: A sudden appearance of floaters might be an indication of a retinal or vitreous detachment. Nearsighted people and those who are diabetic are more prone to both floaters and retinal tears. 63% of the population over 70 experience vitreous detachments (10% before then).
If you suddenly see new floaters, see your eye doctor as soon as possible.
I went on a regimen to include the Advanced Eye Vision & Support, Visual Ocuity drops, Hyaluronic Acid, Pellets, etc... (in addition to a few other supplements I've been taking: Ananeoo sublingual vitamins, and last month started on Molecular Hydrogen tablets 3x/day. ).
I'm VERY PSYCHED to report to you that my last retina appointment was EXCELLENT! No new tears (he had lasered a small retinal tear over 1.5 years ago). His words: "You are doing great!" He doesn't want to see me for a year! I actually asked for a 10 month follow-up, because I was too nervous to go an entire year without seeing him. LOL. He does not advise a vitrectomy if I can "bear the floaters..." I told him I can deal... ??
He gave me the all-clear to get a new eyeglass RX, which I did a couple days later, and another happy surprise! My RX is considerably improved! AND, the optometrist who gave me the new RX also said that she was absolutely convinced that the nutrition is helping. She said that she never sees improvement like this without learning that her patient has been on a nutrition regimen.
Kathy T. June 2024
Related Conditions & Phenomena
- "Scheerer's phenomenon," - small bright dots, lasting for less than a second, which are often seen when looking at the sky. These are actually white blood cells in the retina's capillaries, whose color do not absorb the blue light and therefore are visible as white specks.
- Vitreous detachment
- Premacular bursa is one kind of floater-like experience that appears most often in teenagers and younger adults. Although it looks like a kind of translucent web or area, 'floater' in the premacular bursa are not really floater, because they are not within the vitreous. They are located above the retina in the premacular bursa. They are of microscopic size and appear large only because they are very close to the retina.
Floaters News
Want to learn more? See our blog news on floaters.
 See
Vitamins
& Supplements to support the health of the vitreous.
See
Vitamins
& Supplements to support the health of the vitreous.
Footnotes
1. Alipour, F., Jabbarvand, M., Hashemian, H., Hosseini, S., Khodaparast, M. (2015). Hinged Capsulotomy – Does it Decrease Floaters After Yttrium Aluminum Garnet Laser Capsulotomy? Middle East Afr J Ophthalmol. Jul-Sep; 22(3): 352–355.
2. M.A. Babizhayev, Potentiation of intraocular absorption and drug metabolism of N-acetylcarnosine lubricant eye drops: drug interaction with sight threatening lipid peroxides in the treatment for age-related eye diseases, Drug Metabolism and Drug Interactions, Vol. 24, 2009.
3. M.S. Macedo, Bilateral proliferative retinopathy as the initial presentation of chronic myeloid leukemia, Middle East African Journal of Ophthalmology, October-December, 2013.
4. Milston, R., Madigan, M.C., Sebag, J. (2016). Vitreous floaters: Etiology, diagnostics, and management. Surv Ophthalmol, Mar-Apr;61(2):211-27.
5. Flammer, J., Konieczka, K., Bruno, R.M., Virdis, A., Flammer, A.J., et al. (2013). The eye and the heart. Eur Heart J, May 1; 34(17): 1270-1278.
6. Lyle, W.M., Hopkins, G.A. (1977). The unwanted ocular effects from topical ophthalmic drugs. Their occurrence, avoidance and reversal. J Am Optom Assoc. Dec;48(12):1519-23.
7. Oken, E., Bellinger, D.C. (2008). Fish consumption, methylmercury and child neurodevelopment. Curr Opin Pediatr, Apr; 20(2):178-83.
 info@naturaleyecare.com
info@naturaleyecare.com



 Home
Home


 Vision
Vision Vision
Vision



 Health
Health Health
Health Research/Services
Research/Services Pets
Pets About/Contact
About/Contact


