Macular Hole
Vitamins/supplements Types/progression Symptoms Causes Treatment
A macular hole is a small hole in the center of the retina, the macula. The macula provides the sharp, central vision we need for reading, driving, and seeing fine detail. When a hole develops in the macula, central vision can become distorted or darkened and potentially, over time, lost if not treated.
 See
nutritional support information
See
nutritional support information
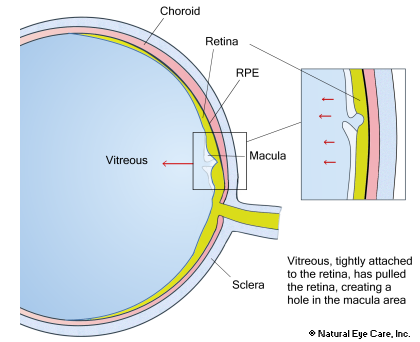
The eye contains a jelly-like substance called the vitreous. With age, the vitreous contracts and pulls away from the retina surface. Usually, this separation occurs without noticeable negative effect. The patient might notice floaters but there is no significant visual damage.
For some people, however, in spots where the vitreous is firmly attached to the retina surface, pulling can occur on the retina, and a small hole may eventually form in the macula. In addition, as we age the vitreous fluid becomes more liquid and less gel-like. It can readily seep through the resulting defect and cause a dark spot or defect in the patient's central vision noticed through distortion and loss of central vision.
Types of Macular Holes
Trauma-Related Macular Hole
Trauma-caused macular holes are thought to be linked to a concussive blow delivered from the opposite site of the head. As a result, the macula ruptures at its thinnest point. 1
Idiopathic-Related Macular Hole
The retina is connected tightly to the vitreous, a layer surrounding the interior of the eye that is filled with vitreous gel. The vitreous is constructed of millions of very fine intertwined fibers. As we age, the vitreous gel begins to liquefy and/or clump and shrink. Idiopathic macular holes are caused by pulling of the vitreous to the side (at a tangent) as the gel and vitreous sac contracts. The retina is attached to the vitreous, and when the vitreous shrinks, it pulls the retina and creates a hole at the thinnest part of the macula. Both retinal and vitreous detachments are aggravated by the contracting vitreous. There are four stages of idiopathic macular holes. Each stage has distinct visual characteristics that allow an eye doctor to identify the severity in an eye exam.2
Stage 1a. Foveal elevation. The fovea is a slight depression in the retina where the center of vision is focused. It is colored yellow, due to the concentration of carotenoid pigments located there. This first stage is, therefore, often called the yellow-dot stage, because the yellow color becomes more prominent.
Stage 1b. Foveal detachment. The foveal part of the retina raises to the level of surrounding tissue, and the yellow dot changes to a yellow doughnut shaped ring around the fovea. Continued pulling leads to rupture of the deeper layers of the retina at the raised fovea. Fifty percent of cases may improve without treatment in stages 1a and 1b.
Stage 2. Partial-thickness hole. The hole is less than 400 microns in size. This is actually a full thickness hole, but there may be a thin cap or top layer that is raised but still partly attached. In stage 2 macular holes, about 70% of cases will worsen without treatment.
Stage 3. Full-thickness hole. A full thickness hole exists, the top cap (pseudo-operculum) has fallen away. The hole is greater than 400 microns in size, and it is still being pulled by the contracted vitreous. This phase causes severe central vision loss.
Stage 4. Full-thickness hole and complete vitreous detachment. A thin shell of vitreous may remain to contribute to the enlargement of the hole.
Symptoms
The severity of the symptoms is dependent on whether the hole is partial or full-thickness.
- Distorted, wavy vision
- Blurred central vision
- Difficulty in detail tasks such as reading
- Central blind spot or gray area
Causes
There have been a few studies to determine the causes and distribution of macular holes, and a few risk factors have been suggested, such as cardiovascular disease, hypertension, and hysterectomy, but none of these risks were statistically significant. Trauma or injury to the eye causes a macular hole less than 10% of the time. Usually these holes seem to develop spontaneously. The medical term describing this type of development is idiopathic, which means the cause is unknown. There may be other factors. Researchers have reported cases of macular hole formation after complete posterior vitreous detachment and vitrectomy. Other theories have been proposed such as a fluid-flow theory. Despite the prevalence of this condition in women, no clear associations have been made.
Conventional Treatment
Surgery is often used to treat severe macular holes. A vitrectomy may treat holes going all the way through the macula. Internal membrane peeling is another technique. Both may result in complications. Read more.
Complementary Treatment
While surgery is generally considered necessary at a certain stage of macular hole progress, with good nutrition we may prevent connective tissue impairments. About 50% of "stage 1" macular holes can heal by themselves. Targeted supplements, along with a healthy diet and regular exercise, can nourish the retina, and support the body's natural healing process. For those that may be prone to macular holes, especially nearsighted seniors, targeted supplements can help keep the retina strong and healthy.
- Certain nutrients, vitamins and enzymes, and fish oil may help recovery from a macular hole. Nutrient recommendations.
- Healthy vision support
recommendations with detailed information.
- Some studies indicate that regular use of Microcurrent Stimulation (MCS) may help preserve vision as well.
from a customer ...
I thought I'd take the time to let you that with your supplements and acupuncture I've been able to close the hole in my eye.
There were three measurements and the progressive trend went as follows
June 2014 > 239 microns
January 2015 > 66 microns
May 15th 2015 > the hole has closed ... I will have to fill in behind the closure for the thickness of the macular membrane ... I'm guessing +/-30 microns or so.
Thanks again.
Ted C., Sarnia, ON., May, 2015
Macular Hole News
Want to learn more? See our blog news on macular holes.
 See
Vitamins & Supplements to
support the connective tissue of the retina.
See
Vitamins & Supplements to
support the connective tissue of the retina.
Research and Footnotes
Though there are no specific studies on nutrients and this particular condition, there is extensive research on nutrients such as lutein, zeaxanthin and bilberry among others that have been shown to be essential for the health of the macula. Based on these studies, Dr. Grossman has selected specific nutrients and products to help support the macula and overall eye health. Some of the research on macular degeneration may be applicable.
Footnotes
1. Medscape. Macular Hole. Retrieved Feb 20 2018 from https://emedicine.medscape.com/article/1224320-overview
2. Johnson, R.N., Gass, J.R. (1988). Idiopathic macular holes. Observations, stages of formation, and implications for surgical intervention. Opthalmology, Jul 95(7):917-24.
 info@naturaleyecare.com
info@naturaleyecare.com



 Home
Home


 Vision
Vision Vision
Vision



 Health
Health Health
Health Research/Services
Research/Services Pets
Pets About/Contact
About/Contact


